
New breakthroughs could ensure more women survive pregnancy and childbirth.
In February, I was with my daughter, Jenn, when she gave birth to a daughter of her own. Welling up
inside me were all the emotions a new grandparent feels: joy, excitement, pride—and, above all, immense gratitude.
In the best of circumstances, childbirth is an exhausting, emotional experience, something I knew from my own experience. It felt like just yesterday that I was giving birth to Jenn in a 14-hour labor that left me utterly drained and barely able to walk.
But in the worst of circumstances, childbirth isn’t just draining—it’s deadly, for mother and baby. Several years ago, I traveled to Malawi, where almost everyone I met had lost someone they loved. At a maternity clinic, the staff, dazed with grief, told me that just the week before, one of their own nurses had given birth, and they couldn’t save her.
I’ll never forget the pain I saw on their faces as they told me about the women they’d lost. The worst part is, so many of these deaths could have been prevented.
For nearly all of human history, we simply didn’t know enough about preventing or treating the common childbirth complications that lead to death, such as postpartum hemorrhage or infection. Today, we know a great deal. Yet, as is so often the case in global health, innovations aren’t making their way to the people who need them most: women in low-income countries like Malawi, as well as Black and Indigenous women in high-income countries like the United States, who are dying at three times the rate of white women, even when holding for economic and education levels.
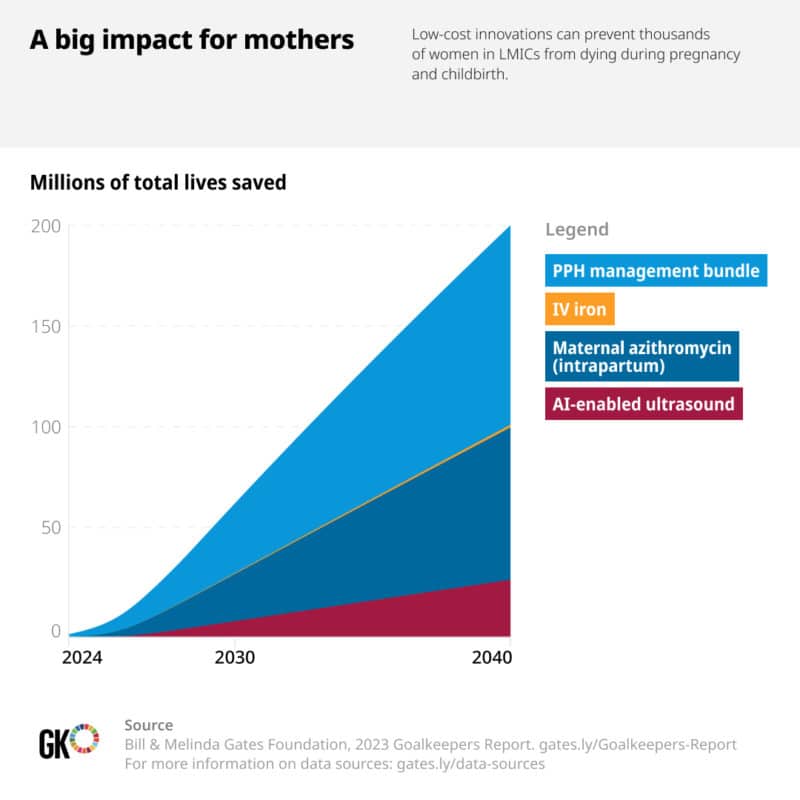
Brilliant researchers have developed new interventions that could ensure more women have access to lifesaving care. Their work is opening up new—and, importantly, low-cost and mobile—avenues of preventing and treating deadly childbirth complications. When combined with better primary health care and more resilient health systems, the three innovations that follow have the potential to save thousands of mothers’ lives in LMICs around the world by 2030.
Here’s how.
Treating postpartum hemorrhage
Postpartum hemorrhage (PPH) is the number one cause of maternal death. The World Health Organization estimates that PPH, which means losing more than half a liter of blood within 24 hours of childbirth, affects 14 million women every year—killing 70,000 of them, primarily in low-income countries. Those who survive often face long-term, disabling complications, such as heart or kidney failure.
Dr. Hadiza Galadanci, an obstetrician and researcher from Nigeria, explains that there is a critical flaw in the way PPH is diagnosed: Health care workers often have a hard time recognizing how much blood loss is too much blood loss. The only tool they have is a rough visual estimate. In a study they called E-MOTIVE, Dr. Galadanci and a team of researchers in four African countries with high maternal mortality found that about half of the women who experience PPH were never diagnosed at all. Therefore, they never got lifesaving treatment.
There is a simple, low-cost way to identify when blood loss is dangerously excessive: a drape that looks like a V-shaped plastic bag. When this calibrated obstetric drape is hung at the edge of the bed, collected blood rises like mercury in a thermometer. And in a busy hospital ward, that visual gauge tells providers which patients are in danger in just a single glance.
When PPH is identified, doctors, nurses, and midwives have long relied on a series of five treatments to stop the bleeding: uterine massage, oxytocic drugs, tranexamic acid, IV fluids, and genital-tract examination. But those interventions were being delivered sequentially—and far too slowly. So the researchers asked providers to bundle the interventions, administering all five at once.
The results were dramatic: In a trial of 200,000 women, providers who used drapes and followed the updated E-MOTIVE guidelines were able to decrease cases of severe bleeding by a remarkable 60 percent.
Preventing PPH in the first place
A common cause of postpartum hemorrhage is anemia, or severe iron deficiency.
Anemia affects as many as 37 percent of pregnant women around the world. In some places in South Asia, that rate jumps as high as 80 percent. Anemia is a dangerous condition on its own, but it is also deeply intertwined with PPH: If a woman has severe anemia, she is much more likely to bleed heavily during her delivery. And even worse, because anemia reduces how much oxygen the blood can carry, anemic women cannot survive the same volume of blood loss as nonanemic women. It’s a vicious cycle.
Symptoms of anemia include fatigue or feeling faint or dizzy—things that might happen simply because you’re pregnant. Every pregnant woman should have access to maternal micronutrient supplements—high-quality prenatal vitamins that include iron—which can prevent most mild maternal anemia cases. But diagnosis and targeted treatment are necessary to address moderate and severe cases of anemia. So once again, a primary challenge is diagnosis. Screening for anemia during pregnancy is one of the most important tests we can do to ensure a woman’s health and survival. And just one example of why antenatal care is so important.
If anemia is diagnosed, the traditional treatment is supplemental iron delivered via tablets. But taking iron orally can cause unpleasant side effects and requires women to keep up with a consistent regimen for up to 180 days.
But a Nigerian obstetrician and researcher named Dr. Bosede Afolabi is working on bringing a promising new intervention to her home country: a one-time, 15-minute intravenous (IV) infusion of iron. It’s an IV drip that can replenish women’s iron reserves during pregnancy—or even after pregnancy—and it could help treat severe cases of anemia quickly and effectively.
Anemia isn’t just a cause of postpartum hemorrhage; it’s also an effect—one that can lead to long-term consequences ranging from heart disease to depression. So this solution could mean not just saving women’s lives but also helping them lead better ones.
Preventing infections
Another leading cause of maternal death and disability is infection that leads to sepsis—an extreme, full-body inflammatory reaction. In recent years, researchers have discovered that one of the most promising new ways to prevent infection during pregnancy happens to be one of the most commonly used antibiotics in the world.
For decades, azithromycin has been used to treat a variety of bacterial infections, most commonly eye and respiratory infections. Now we’re learning that when given during labor, azithromycin also reduces maternal infections, therefore preventing those infections from spiraling into sepsis. During a trial across sub-Saharan Africa, it reduced sepsis cases by a third. That’s a remarkable discovery—one that could be very useful in places where most births are at home.
And it could also be a game-changer in the United States, where 23 percent of maternal deaths are from sepsis.
The United States has some of the most abysmal—and most inequitable—maternal mortality rates among high-income countries. American women are more than three times more likely to die from childbirth than women in almost every other wealthy country. But, as I noted earlier, the biggest crisis is among Black and Indigenous women.
I still remember the shock I felt when I read tennis star Serena Williams’s account of how close she came to dying from serious blood clots after giving birth—simply because her own doctors wouldn’t believe her that something was wrong. That shock only grew when I read, just this past April, that Tori Bowie, a Black American track and field Olympian, died from childbirth complications in her home. And these are just the stories we hear about in headlines.
It’s remarkable that a common antibiotic like azithromycin has the potential to address the cause of nearly a quarter of American maternal deaths.
But as Serena’s harrowing experience and Tori’s tragic death demonstrate, one antibiotic is not enough. The systemic inequalities that deny the highest-quality care to Black and Indigenous women also need to be addressed—urgently.
A powerful engine for progress
These are three of the innovations that are reshaping maternal health—and there are others just on the horizon, especially as researchers learn more about how to use AI to improve maternal health care.
Of course, these breakthroughs aren’t silver bullets on their own—they require countries to keep recruiting, training, and fairly compensating health care workers, especially midwives, and building more resilient health care systems. But together, they can save the lives of thousands of women every year. And that’s not all.
Improving maternal health also means improving infant health and survival. It means stronger families, more vibrant communities, and more prosperous societies. We have seen over and over again that when countries actually prioritize and invest in women’s health, they unleash a powerful engine for progress that can reduce poverty, advance gender equality, and build resilient economies.
“Improving maternal health also means improving infant health and survival. It means stronger families, more vibrant communities, and more prosperous societies.”
—Melinda French Gates
That’s why, more than anything, we need to rally the will to invest in these breakthroughs—so they actually get to the women who need them most—and fund the remarkable researchers who will discover the next ones.
Dr. Afolabi explained that in the Yoruba language, the traditional greeting to a woman who has given birth is “Eku ewu omo,” which translates to, “Well done for getting through the danger of childbirth.”
Thanks to her, and others like her, more women will live long enough to hear those words. And maybe one day, when breakthroughs have reached women all around the world and childbirth is far less dangerous, all they’ll hear is “Well done.”

